Alison Holloran is thankful for what she didn’t know in the moments surrounding her diagnosis with Stage 2 breast cancer. She understood that treatment would be difficult. She knew her life would be forever changed. What she didn’t know—and couldn’t have anticipated—is the difference between “surviving” cancer and healing from the traumas associated with a life-threatening illness.
“I’m glad I didn’t know how hard it would be,” said 47-year-old Holloran, a Fort Collins-area pilates instructor and nonprofit executive director. Diagnosed at age 45, she’s officially cancer-free. Yet she’s still learning how to navigate life after cancer.
Her experience isn’t unusual, says Alene Nitzky, PhD, RN, OCN. “Surviving cancer is just one part a person must go through. Learning how to live—truly live—after cancer is so much more.”
A Surprise Diagnosis
Holloran received her first mammogram at the age of 40. It came back normal, as she suspected.
“I didn’t have any family history of breast cancer, and I was healthy. I had been a pilates instructor for 12 years, I ate relatively well, and I was an avid runner.”
Not long after she had her next mammogram, at age 45, she got a call indicating the mammogram found a small lump in her right breast, deep against her chest wall.

Alison Holloran, Cancer survivor. Photo courtesy of Julie Ulstrup Photography
“I couldn’t help but think, I’m doing everything right…and now this? It was a punch in the gut.”
After more testing, Holloran was diagnosed with Stage 2A cancer. She had surgery to remove her lymph nodes and underwent six months of what she called “hard core” chemotherapy (including two months of doxorubicin, often called “the red devil” because of its serious side effects). She underwent seven weeks of radiation and took medications to stop her body from producing estrogen, as her tumor was the type that could grow in response to her body’s natural production of estrogen. This summer, she had her ovaries removed preventatively, and will continue to take an estrogen-reducing drug called anastrozole every day for five years to stop her body from producing the hormone.
Living Versus Surviving
“When I first started treatment, I thought, I can do this,” said Holloran. She had a great support network of family and friends anxious to do what they could to help.
“But the truth is that I had to learn to ask for help, and that was hard for me. I come from a generation of women who could ‘have it all’—the career, the kids, everything. So, I thought, I can manage this. But you quickly learn that you simply can’t. I never wanted to be a burden, but I really needed the help.”
Becoming Your Own Advocate
“Our health care system isn’t set up to allow someone to heal from an illness,” Holloran explained. “I had a staph infection but was told it was a ‘normal’ side effect. But I knew something else was wrong. I finally saw a dermatologist who instantly diagnosed me, but I suffered for six months. You’ve got to be your own best advocate!”
At another point, insurance denied coverage for a treatment her doctor deemed necessary. “I offered to pay out of pocket and learned a single dose cost $40,000.”
Eventually insurance covered the cost. But Holloran is still recovering financially.
“I’m still fighting my insurance company over a $4,000 bill.”
Post-Treatment Support
Nitzky no longer works as an oncology nurse. Now she develops programs that help cancer survivors thrive post-treatment. Her programs focus on self-care and advocacy, because at the end of the day, it’s on the individual to own her own healing.
“Patients and their families expect them to bounce back immediately after treatment,” Nitzky explained. “But the residual effects linger. Most deal with extreme fatigue, as well as anxiety and depression. They don’t understand what ‘self-care’ means, and how to care for yourself at work, home, and in leisure settings.”
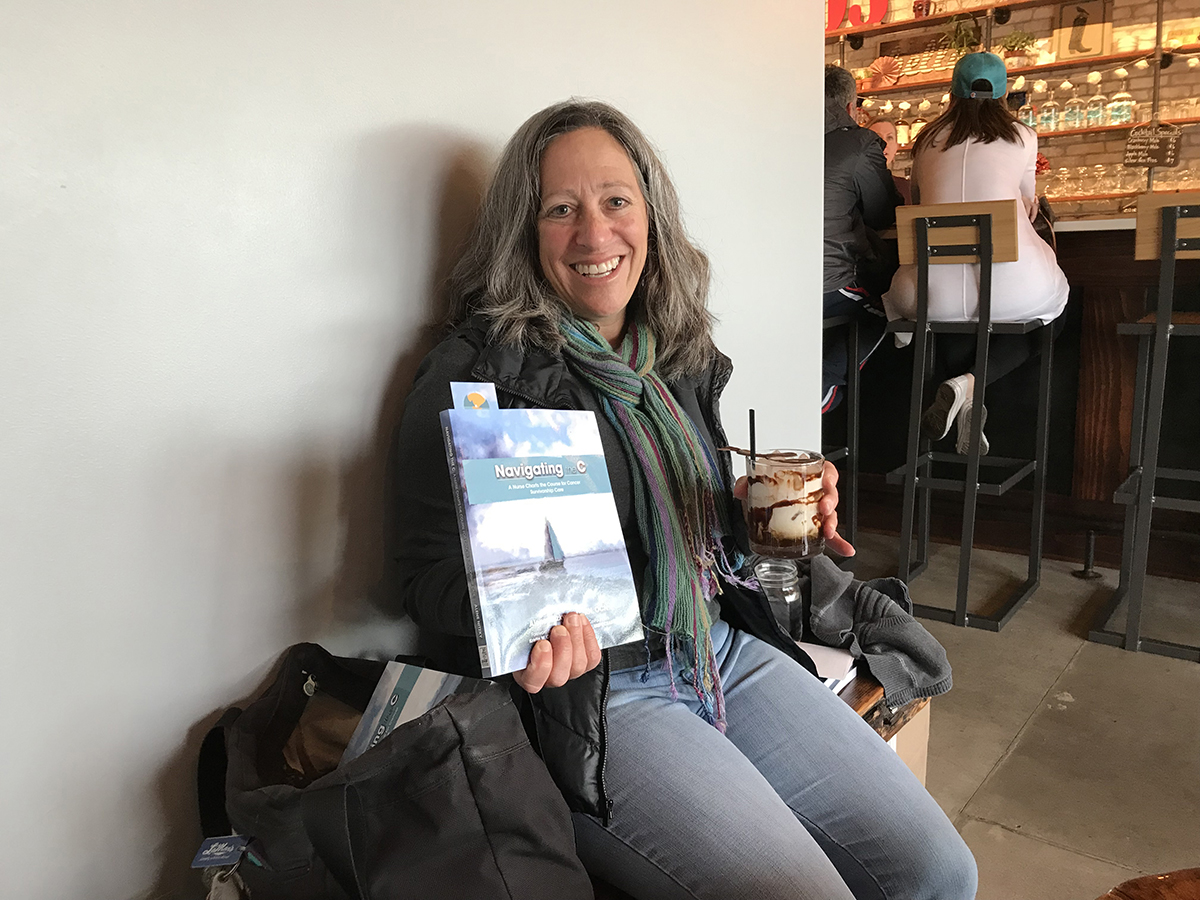
Oncology nurse and author of Navigating the C, Alene Nitzky now develops post-treatment programs for cancer survivors.
Post-treatment, Holloran found herself at a loss for what to do next.
“After you go through the struggle of treatment, you think it’s over. But that’s the moment where the work really begins. How am I going to change so this cancer doesn’t come back? How do I move forward with life, moving forward? It took going to counseling to help me understand all of this.”
Holloran thought she understood self-care before she got sick.
“Cancer forced me to take a hard look at my life,” she said. “I didn’t get sick because a lightning bolt hit me. I was always busy, always ‘on,’ always feeling stressed. I was always telling my pilates clients to ‘listen to your body,’ yet I wasn’t doing the same.”
Although her journey hasn’t been easy, Holloran has grown because of it.
“Physically, I have a better appreciation for all that I have. I have a different perspective on stress. Looking back, that’s a really good thing.”

How Family and Friends Can Help
Someone you love has been diagnosed with cancer. Now what?
Do something. Anything. “Everyone always ask, ‘what can I do?’” said Holloran. “But when you’re sick, you don’t want to be a burden. So, don’t ask. Bring a meal for the freezer. Stop by for a visit. Drive your friend to an appointment. Just do something.”
Educate yourself. “It helps everyone to know a little bit about cancer,” said Nitzky. “Most people hear the word cancer and instantly think of death. Yes, people still die from cancer, but it’s nothing like it used to be. When we as supporters react from our own fear, we become less able to listen and empathize with our friend or family member.”
Connect with community resources. “Here in Fort Collins, there’s an organization called Hope Lives that connects cancer survivors to resources,” said Nitzky. Says Holloran, “Hope Lives is so great. I can go to counseling and to an acupuncturist for my frozen shoulder, for free.”
What the Experts Say
On mammograms. There’s conflicting advice. “Generally speaking, women should have their first mammogram at age 40, with repeat mammograms annually thereafter,” says Molly Decker, DO, chair of surgery at Banner Northern Colorado Medical Center and regional lead, surgical oncology at Banner MD Anderson Colorado. In 3-D? Women are sometimes offered a 3-D mammogram; however, insurance doesn’t always cover these. “We typically reserve 3-D mammograms for cases in which we’ve seen something on the original mammogram that might be abnormal,” says Decker. “We would typically call the patient back for a 3-D mammogram to better delineate.”
Self-exams. “This is a hot topic,” says Decker. “And it’s a difficult question to answer. We used to encourage them, but studies found that we were finding more benign breast disease in young women without diagnosing more cancer. I recommend women have an annual clinical breast exam by their primary care or OB/GYN, though if you have a family history or you’re postmenopausal, monthly self-exams may be of benefit.”
Bottom line. If you’re diagnosed, know that outcomes are very good. “Treatment won’t be a walk in the park, but our rates of survivorship are excellent, and rates of recurrence are relatively low. Most women go on to live a long, happy life.”
Cancer: By the Numbers
25,570 Estimated number of new cases of cancer diagnosed in Colorado in 2018
1 in 10 Number of women screened who have an abnormal mammogram; 5 percent of these turn out to have cancer
9,320 Estimated deaths from melanoma, the most common form of cancer in the United States, in 2018
Source: American Cancer Society
Carie Sherman is a Denver-based freelance writer. To comment on this article, send an email to letters@nocostyle.com.