Julie Rojas’ office has the standard rubber gloves, a table and plenty of other tools for patient care, but it doesn’t look like an examination room. That’s precisely the point.
There are coloring books (the kind to occupy little kids) stacked on a shelf. On a wall a few inches from the rubber gloves is a sign with the word “human” in white letters with rainbow stripes. There’s a calendar with dogs and cats. It smells nice, not antiseptic. It’s a room ready to treat trauma patients thoroughly but with compassion.
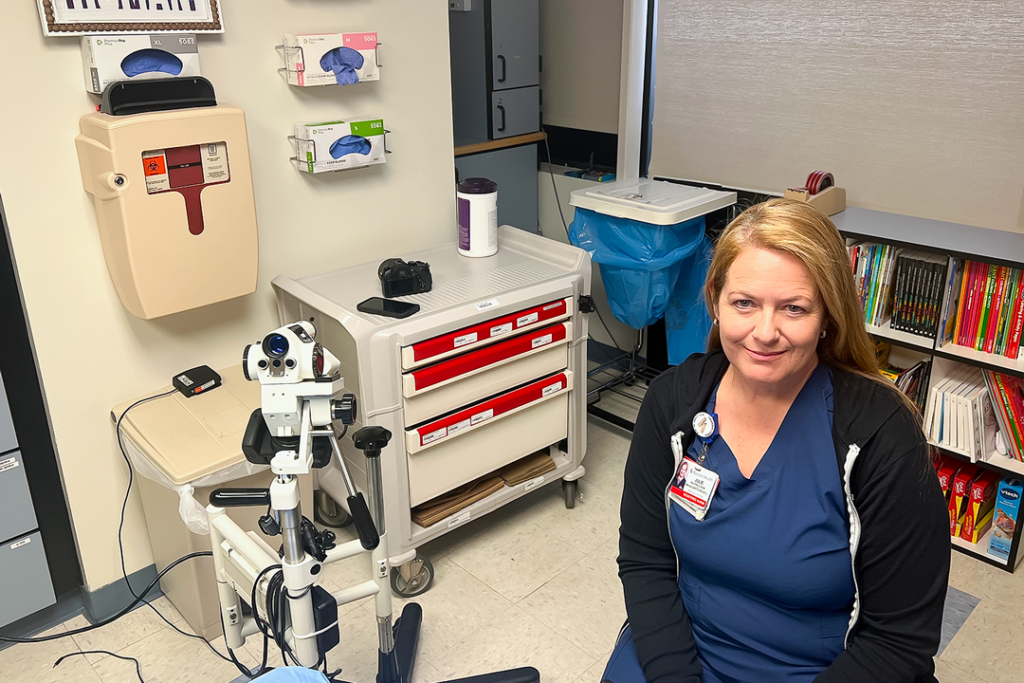
Julie Rojas
Rojas treats many survivors of assault and abuse. There are, as you can imagine, a lot of hard cases mixed in with the bar fights. She cares for rape survivors and commonly sees signs of long-term abuse in children, the elderly and domestic partners. She treats people who are probably being trafficked. She sees more trauma in a day than most of us would see in a lifetime.
Rojas works as a forensic nurse at Banner North Colorado Medical Center in Greeley. She calls it her dream job, even though, when her husband asks about her day, she only tells him whether it was good or bad. She doesn’t give details, and he doesn’t want to hear them.
Rojas loves her job because, in her words, she can really care for her patients, a luxury most nurses don’t get anymore.
“You can spend as much time as you need with one person,” Rojas says. “That’s a dream. They want you in there.”
Forensic nurses specialize in compassionate, straight-forward, non-judgmental care while offering to collect evidence, find resources and, at times, help patients escape dangerous situations. These nurses undergo a year of additional training and 64 hours of free classes before stepping into the role.
Banner Health and other hospitals, including UCHealth, don’t charge patients who are treated by trauma nurses. Doing so, Rojas says, wouldn’t be fair and would potentially deter them from seeking care. Some funding comes from the state and local police departments, but hospitals cover the rest. That’s part of the reason why Rojas believes in what she does.
“It’s like a social service,” she says.
It’s also not the time for competition. Rojas texts nurses at UCHealth daily to talk about specific cases and how to handle them. This communication helps to ensure that patient care remains consistent.
“We are really big on doing things the same way so the patients have a choice on where to go,” says Michelle Breese, the forensic nursing coordinator in UCHealth’s Northern Colorado region. “We want this care to look the same way.”
Nurses from both hospitals help each other through even the toughest cases, Breese says, in the same way police officers will talk things out amongst themselves. Breese would know: She worked in law enforcement prior to becoming a nurse.

Michelle Breese
“You have to be really passionate about this,” she says. “When you are passionate, you’re willing to work through those challenges.”
Breese likes being a nurse better than being a cop, though she doesn’t see much difference between the two.
“The only real difference is that I don’t have to worry about the legal part of it,” she says. “I don’t have to worry about the bad guy. I’m just giving holistic care to my patient.”
Forensic nurses work hard to give their patients back the power that’s been taken from them. They never call them victims. They also won’t do anything without their patients’ permission during the examination, and that includes patients being questioned by the cops.
They don’t put pressure on patients to report their cases or seek help, but they do warn them about specific instances of abuse, like strangulation. People willing to do that are seven times more likely to kill, Rojas says.
Patients don’t have to press charges or have any contact with the police at all. They’re at the hospital for treatment, not to face questioning from officers. The evidence the nurses collect (if patients allow it) stays in the hospital, giving them time to decide what to do. Some patients will press charges after a year or longer, Rojas says.
“We consider it planting a seed,” she says.
The need for this type of care is always there. One in three women and one in six men will experience sexual assault in their lifetime, according to Banner. And though Rojas may see more marginalized people, assault and abuse are issues experienced by people of all ages, races, genders, sexual orientations, economic classes and income levels.
However, she does see more patients when college students come back for the school year and find themselves in more vulnerable positions, as well as during the holidays.
The number of patients treated by Banner forensic nurses has increased as well. When the program started nearly a decade ago, Banner’s NCMC Rehabilitation Center saw 64 patients the first year. In 2022, there were more than 300. UCHealth projects that its forensic nurses will treat 1,000 patients in its six emergency rooms throughout Northern Colorado this year.
The nurses see the growing numbers as a good thing. They don’t wish the trauma on anyone, but they want to be there for them when it happens.
“It’s probably the most traumatic part of their lives they’ve ever been through,” Breese says. “But you can get care and move forward from these events. That’s the part of nursing that I really love the most.”